
Table of Contents
Overview
1.
Organizations are competing for the same pool of people, but on different terms
2.
Recruiting is getting more strategic by necessity
3.
Under-preparation is leading to burnout in new graduates
4.
Therapists are becoming risk averse – and it can affect care quality
5.
Mental health may be heading towards being a 24/7 profession
6.
Supervision is both a recruiting and a retention tactic
7.
Organizations need trained managers but struggle to deliver
8.
Rather than fight attrition, CMHCs are designing for it
9.
Private practice looks greener but may not be
10.
We cannot adequately support the next generation of therapists
Conclusion
Workforce Trends: Behavioral Health in Focus
We’re so excited to invite you to read our report on some of the emerging trends in clinical and professional development for therapists. Our goal in creating it was to uncover the key drivers and challenges that therapists face, so that we’re better equipped to support the next generation. Drawing on real, lived experiences, this report captures the voices of professionals navigating today’s challenging mental health landscape to deliver insights from the front line.
We talked to numerous professionals – both clinical and managerial – at mental health organizations ranging from small non-profit all the way to large corporate. These in-depth discussions allowed us to identify trends and also understand context, subtext and a complex set of motivations. Several of our interviewees agreed to let us reference them in this report; We’ve relied heavily on their personal quotes to most accurately convey their direct observations and experiences. For those who preferred to stay anonymous, we’ve used their input to shape the overall narrative. Please note: this report represents the insights of the people we talked to, and not necessarily of their organizations.
Although this report doesn’t include quantitative data, it provides a snapshot of real-time trends that are shaping the supply side of mental healthcare. We hope these insights will resonate with you, and help you respond to the evolving needs and expectations of the communities you serve.


Rachel Ledbetter, LMFT
Overview
Much has been written about the skyrocketing demand for mental health services. We took on this project to understand the supply side of mental health, with a fundamental question:
How are organizations addressing the fact that demand for services is rapidly outpacing the availability of therapists?
We found that organizations across the behavioral health industry are responding with innovative approaches to clinical and professional development to improve both the supply and quality of mental health providers.
But it’s a case of stark contrasts.
Experienced therapists have a range of employment options, while new associates—graduating in large numbers—are historically drawn to community mental health centers to secure the supervised hours they need for licensure.
These associates are getting trained in under-resourced environments, overseen by overburdened supervisors, some of whom lack the experience or capacity for effective mentorship. Then, we put these new graduates in front of the most complex cases with minimal support, leading to early burnout.
It’s no wonder 57% of these new graduates never attain licensure.
Most therapists enter the field to help others and make a meaningful difference in the world. Yet the system can leave them feeling undervalued and exploited.
We do actual harm to clinicians through inadequate training and supervision, and by not providing them with some of the basic benefits that most people enjoy in their job like experienced management, a safe work environment, and reasonable hours.
This is not a sustainable model for success. If we want the mental health profession to thrive, we need to make significant changes that truly support and empower clinicians.
1.
Organizations are Competing for the Same Pool of People – but on Different Terms
According to recent data released by the US Bureau of Labor Statistics, mental health jobs are growing at a rate that’s three times higher than the rate for most other industries. Jobs that address substance abuse and behavioral disorders are projected to grow even more rapidly over the next ten years.
At the same time, therapists are leaving their place of employment at turnover rates as high as 30-60%, compromising quality and consistency of care and depressing therapist morale across the industry.
The net effect: Supply is not growing at a pace to keep up with demand. As a result, mental health organizations are all competing for the same limited pool of therapists, making recruiting a constant and relentless struggle.
But they’re not competing on the same grounds.
Models of mental health organizations differ in terms of why clinicians join them and why they leave. This gives employers a basis to be more strategic in their selection and retention of candidates and seek out people who align with their mission, benefits, and work environments.
Community Health
Why people join
- Intensive hands-on training
- Ample client hours
- Free clinical supervision
- Ability to help people who would otherwise not get help
Why they are leaving
Low pay and benefits
Hard(er) working conditions (hours, patient acuity, safety concerns)
- Less predictable schedule
- Tighter capacity – fewer resources, longer waiting lists
Private Hospitals / Collaborative Care
Why people join
- Team-based approach (“whole person”)
- Perks and benefits
- Organized training and career management
- Access to resources (e.g., technology / AI)
Why they are leaving
- Fast-paced work environment
- Behavioral health may be considered supplemental to physical care
- High patient acuity
- Lack of flexibility
Private Virtual Health Companies
Why people join
- Virtual care / Work at home if desired
- Perks and benefits
- Organized training and career management
- Access to resources (e.g., technology / AI)
Why they are leaving
- Investor pressure on performance and profitability
- Ethical concerns
- Low pay per hour
Private Practice
Why people join
- Autonomy over their practice
- Flexible schedule
- More opportunity for virtual care / work at home if desired
- Higher pay per session
Why they are leaving
- No stable salary; no benefits; no vacation time
- Hard to get credentialed with insurance
- No administrative support
- Lack of community
2.
Recruiting is Getting More Strategic by Necessity

Recruiting (into community health) has gotten so much harder. The acuity level has increased, so people are struggling more. Recruiting for us means finding someone who can not only handle serious persistent mental illness – SPMI – but who is also able to keep up with their billable hours and handle the never-ending documentation, which has absolutely increased.

Carla Myers, MS, LPC, MHSP
Former Clinical Director, Bridge Health
Recruiting in behavioral health faces significant challenges. A shrinking candidate pool and increasingly difficult work conditions make positions harder to fill. Traditional recruitment approaches are proving less effective, leading organizations to explore innovative strategies to attract and retain talent more successfully.
It’s the opposite with pre-licensed therapists, who don’t have similar choices, and instead, go wherever they have a path to licensure.
Peer-to-Peer Recruiting
We had a recruitment problem for the first five years of the behavioral program. We were using our usual talent acquisition department – but they didn’t really know about behavioral health, they didn’t know how to speak about the program. Within the first nine months of 2023, we had five different recruiters working on behavioral health for us, and it wasn’t working. We then decided to flip our recruitment out of talent acquisition and into provider services, which recruits for our primary care physicians. So they now recruit for any clinical provider at the organization. Then we took one of our actual behavioral health specialists, an LCSW, who was looking for the next leg of her career, and had her become a recruiter. She has taken us from 90 BH specialists to 130 in eight months. She’s really talented at finding individual. We also spend a lot of money towards marketing the different roles we have, particularly on LinkedIn. But importantly, she’s able to speak to the program as a former clinician in the program, and that works to woo these clinicians to come to us.

Rebecca Murray, LCSW
Senior Clinical Director of Behavioral Health, Oak Street Health
Peer-to-Peer Recruiting Requires a Special Kind of Skill Set
We’ve found that peer recruiting can be very successful as long as the therapist has the mindset and skill set of a recruiter, because a therapist recruiter role is very different. You have to be OK with rejection, you have to be OK with people saying no to you a lot, you need to go through the grind while being able to empathetically share your experience as a therapist.

Michelle Turner
Vice President, Clinical Talent and Delivery, Hazel Health

Community Relations
We’ve done a lot of targeted sourcing and have built relationships with associations and organizations in our key states. We put on webinars and participate in speaking engagements and help provide education. Our clinical leaders share with their clinical leaders so we are truly collaborating and not just seen as outsiders. We have tried to lay the groundwork for a long-term relationship that is mutually beneficial.

Michelle Turner
Vice President, Clinical Talent and Delivery, Hazel Health
Staffing Peer/Community Support Roles
I think that there needs to be more focus on reducing the burden on the clinician so that the clinician can focus on what they do best, which is providing therapy. So subclinical roles like behavior coaches, community health workers and peer-to-peer specialists have to be a part of the solution. Most of the Medicaid-serving community mental health organizations already assign a clinician to focus on therapy and mental health symptoms, and a case manager to help people with their resume, get ready for interviews, create a chore chart for their kids to create more structure. Those are bachelor’s or high school level people that are billing too. I think peer support is another service – which is someone who has lived experience with substance abuse or mental illness that is also assigned to the case to be a buddy, talking to you as a peer. This has proven to be very effective. However, many organizations struggle to find and train peers for this role – and the reimbursement rate is quite low.

Rachel Ledbetter, LMFT
CEO & Co-founder, Motivo Health
Motivo Job Match
Motivo created Motivo Job Match™ to bridge behavioral health providers with job seekers. To operationalize this new service, Motivo is leveraging its existing relationships with behavioral health employers and establishing new partnerships with universities. The company has expanded its secure supervision platform to now include recruiting services, effectively connecting these key constituents.
Behavioral health providers using Motivo Job Match™ will also have access to Motivo’s network of supervisors to provide virtual supervision for the pre-licensed therapists they hire, and help coordinate their completion of licensure requirements. Motivo Job Match™ participants will also have access to continuing education and a bi-weekly peer support group facilitated by the Motivo clinical leadership team.
3.
Under-Preparation is Leading to Burnout in New Graduates

We’re seeing more people than I’ve ever seen leave their profession, and leave it soon after they graduate. So it isn’t like, I’ve been doing patient care for 10 years and I’m out; they’re leaving very soon following graduation.

Virna Little, PsyD, LCSW-R
Co-Founder, Concert Health
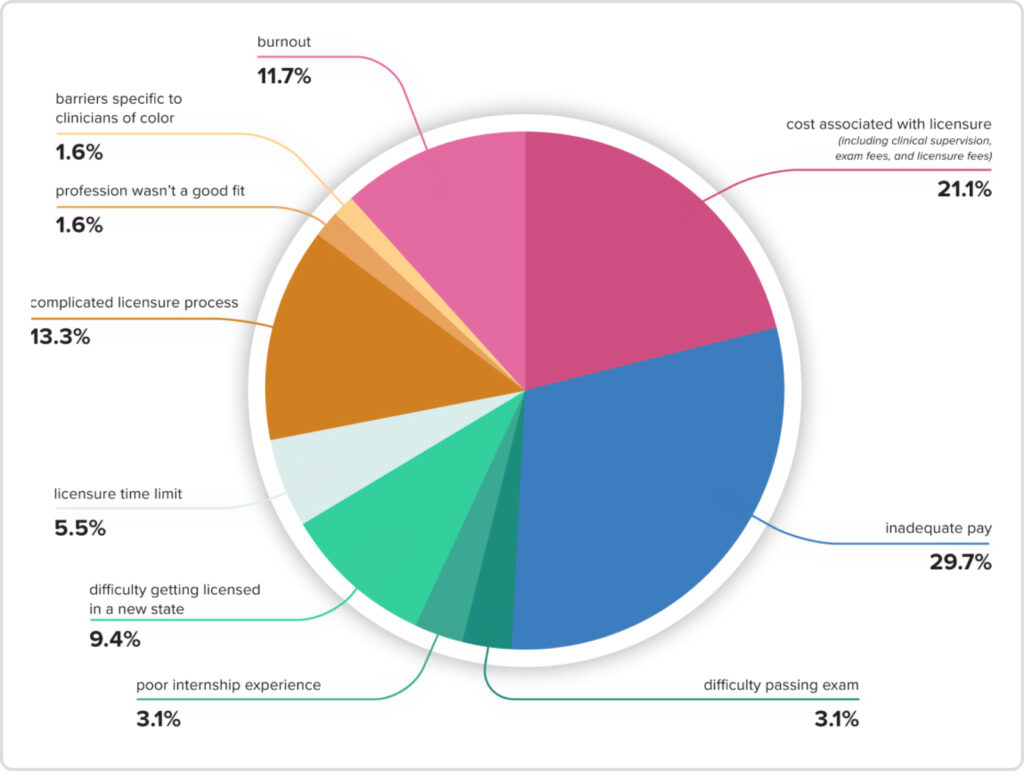
A staggering 57% of pre-licensed clinicians leave the profession before even becoming licensed. While much of that attrition has to do with the cost and complexity of licensure, many new graduates are leaving the profession because of reasons related to burnout or the inability to manage the job’s expectations.
How is someone burned out on their career before it has even begun?
We learned that new graduates are not being adequately prepared for a career in mental health. And this under-preparation is leading to a crisis of confidence among our newest therapists, and is driving attrition.
Universities are Underperforming
The schools are moving away from teaching students the skills that they actually need. I had a conversation with a school the other day that took out the diagnostic classes and some of that instruction from their curriculum. So when these people graduate, they’re going to get put in a community mental health center and they’re going to have to diagnose people and treat them, and you’re not preparing them for what they need to do.

Virna Little, PsyD, LCSW-R
Co-Founder, Concert Health
Wide Variability in New Therapist Graduate Skills
Our expectation is that schools will prepare their students for practicum and that is not always the case. There’s a dramatically varying level of preparedness for it, that varies widely by school. There are certain schools where the folks coming into practice feel woefully underprepared. Then there are some schools where they’re ready to hit the ground running. It’s a pretty clear distinction. But we take almost everyone; we need as many people as possible.

Adina Ascher, LCSW, PhD
Clinical Director, The Liberation Institute
Mismatch of Expectations
A lot of people think that they’re gonna be Frasier and live in this beautiful apartment in some big city and make tons of money. And it’s not like that. Especially in inpatient facilities, where you’re handling psychoses or violence, and may be called at 2 am.

Carla Myers, MS, LPC, MHSP
Former Clinical Director, Bridge Health

Training By Not Training
Community mental health has a long waitlist of patients to see. I remember a scenario where a mom had children who had been removed from her home because she tested positive on a drug test and she had to participate in counseling in order to get her kids back. Someone like her gets referred to community mental health, and they don’t have a clinician to see her, so she’s waiting for the ability to participate in therapy so that she can get her children back. It’s stressful for the patients, and it’s stressful for the organization because they have these people on their caseload that they can’t even bill for, so it’s missed revenue for them. So pretty much anybody who walks through the door is given a job, it’s like, we just need to get you going. They are not going to say, let’s spend a full day in training so that you know how to provide better care to the Medicaid population. Instead, we’re just throwing our greenest clinicians into the deep end of working with the most vulnerable clients with no training or support or structure. It’s not because these organizations don’t want to do it, it’s because they’re working with high caseloads, long waitlists and shoestring budgets.

Rachel Ledbetter, LMFT
CEO & Co-founder, Motivo Health
Parity in Access but not in Training
We’ve had like 70 years of not investing enough in our mental health system. I think now that we have parity rules and people are more likely to report depression and anxiety and mental health disorders, it’s become a crisis. The population has grown but most of our training programs have not. And many of the people that were in practice are retiring or working part time, not fully participating in the workforce anymore. Essentially, the gap is just widening between the level of need and the amount of providers because we haven’t expanded our training programs. It’s really expensive to train someone well and nobody is willing to pay for it. A lot of people are like, that’s your job to figure out how to get trained and I just expect you to show up trained to my workforce. I personally think the payers are actually responsible for providing an adequate network and I think they should be contributing more to the paying for the training of the workforce. CMS pays for residents, so that model is already out there.

Anna Ratzliff, MD, PhD
Co-Director, AIMS Center, University of Washington
Training in Uncharted Territory
The current generation of therapists is encountering challenges their professors and supervisors never faced. For example, children are now disclosing suicidal thoughts to strangers on platforms like Roblox or to non-mental health AI bots. These are monumental shifts to navigate. Since I got licensed in 2015 – just a decade ago – the landscape of mental health care has transformed in ways we couldn’t have anticipated. Supervisors, clinical leaders, and mentors may not have the direct experience their supervisees and associates now face. This makes it essential for mental health leaders and clinical supervisors to commit to lifelong learning. Engaging in this learning will help us stay attuned to what people are experiencing in real time, with space to consider historical and social contexts – that’s true cultural responsiveness.

Carla Smith, PhD, LCSW, LMFT
Chief Clinical Officer, Motivo
Owner, Haven Therapy and Wellness
Suicide Prevention – a Missing Skill
The evidence-based safety planning intervention was developed by Stanley and Brown. It is not fill-out-a-form; it is actually talk-to-the-patients, have them tell you a narrative of the last time they were at risk for suicide, and based off of that, help them develop a plan to intervene at key places across the chain analysis. But most people don’t deliver it that way. I think what most people are doing these days is filling out a form. It takes a lot of time to train someone to do narrative-based intervention. Every time a provider is spending time training, they’re not seeing patients. And right now there’s so much need to have patient care happen, I think people are like, something’s better than nothing; like, check, you’re good enough on suicide. I don’t mean that people don’t want better, but they’re desperate.

Anna Ratzliff, MD, PhD
Co-Director, AIMS Center, University of Washington
Underprepared, not Burned Out
For new clinicians who are just entering the field or poorly trained clinicians, every time they see a patient, it’s like going on a roller coaster ride because they don’t have the skills to facilitate – or control – the session. Everyday they go on 8 to 10 roller coaster rides, which is exhausting. So, if you have the tools, and you have the training, then you don’t have to go on the ride. You stand on the platform to manage the ride. You’re able to get good outcomes, but it’s a lot less exhausting. By virtue of giving people some training and the skills they need, we can actually reduce some of the burnout and address some of the retention.

Virna Little, PsyD, LCSW-R
Co-Founder, Concert Health

The High Cost of Under-Preparation
I do think there’s a cost that people aren’t talking about. When people aren’t well trained, they then feel less effective in their job, and they actually quit more often. So I think actually we need to be talking about that cost a bit more upfront, because it is morally distressing to not be able to provide good care to people. That leads to burnout and then people are like, well, if I can’t do this job well I’m just going to leave.

Anna Ratzliff, MD, PhD
Co-Director, AIMS Center, University of Washington
Need More Standardization
The entire profession would benefit from reimagining mental health training along the lines of medical residencies. More structured programs, standardized requirements and intensive, real-world experience would teach (new graduates) resilience.

Virna Little, PsyD, LCSW-R
Co-Founder, Concert Health
Suicide Statistics
Many adults think about suicide or attempt suicide.
- 13.2 million seriously thought about suicide
- 3.8 million made a plan for suicide
- 1.6 million attempted suicide
Source: Center of Disease Control
4.
Therapists are Becoming Risk Averse – and It Can Affect Care Quality
Many people we talked to observed that therapists are increasingly becoming risk-averse. Some factors are being felt across professions, like the fear of being perceived as ‘labeling’ people and the fear of being called out on social media. Several factors, however, come from within the profession, and have the potential to compromise our ability to accurately diagnose people and deliver quality care.

Lack of Protection
I think that there’s a general lack of protection for therapists, both physically and professionally. Given the high risk, high acuity nature of mental health issues in many communities, therapists often encounter situations that put their physical safety at risk. On top of that, there’s a significant professional vulnerability: therapists’ licenses lack robust protections, leaving them susceptible to sanctions or disciplinary action due to potential oversights in client care compared to other professions. As a result, many therapists are opting out of these challenging environments and roles, feeling the personal and professional risks simply aren’t worth it. That said, I do believe a great deal of mental health providers are taking their protection into their own hands by utilizing malpractice insurance, additional training, and advocacy efforts where they can.

Carla Smith, PhD, LCSW, LMFT
Chief Clinical Officer, Motivo
Owner, Haven Therapy and Wellness

Medicaid Takebacks
In some states like New Mexico where they’ve had a lot of Medicaid take backs, I think they’ve kind of gone the other direction and they’re so full of risk aversion, and I think that’s part of the problem. We’ve created a whole generation of these mental health organizations that are very risk averse because of the take backs, because of the audits and because of HIPAA and 42 CFR, and so I think that is part of the problem.

Virna Little, PsyD, LCSW-R
Co-Founder, Concert Health
Mental Health Discrimination
Military families are very concerned about diagnosis because they understand it can keep their children from being able to serve later on and that’s a huge thing. We are a military family and I have seen kids who, all their life, wanted to grow up and be in the marines like their dad; and they can’t because in 3rd grade, they had an ADHD diagnosis, and now that meansz when they’re 18 they’re not able to pass the screening requirements to join.

Michelle Turner
Vice President, Clinical Talent and Delivery, Hazel Health
DIY Mental Health
People who are getting mental healthcare are increasingly accessing care advice from social media and non-mental health AI platforms, adding a new layer of complexity for therapists. Therapists find themselves needing to clarify, “My professional training says something different,” as they work with clients heavily influenced by online content. This is similar to what medical doctors face when patients self-diagnose through online sources and request specific treatments or medications accordingly. However, in therapy services – where medications aren’t typically involved and there are fewer guardrails – this issue is even more pronounced. Therapists have little control over these external influences that impact their clients, who may already be in a vulnerable state. Despite this, therapists are still expected to assume responsibility for any adverse effects these outside influences may have on their clients’ well-being.

Carla Smith, PhD, LCSW, LMFT
Chief Clinical Officer, Motivo
Owner, Haven Therapy and Wellness
5.
Mental Health May Be Heading towards Being a 24/7 Profession
Perhaps it’s the rising demand for mental healthcare or the ease of virtual care that’s driving a huge demand for evening therapist appointments. Or perhaps it is the increasing competition in the private sector that’s raising the competitive bar for 24/7 access. But regardless of the reason, there’s a growing expectation that therapists have to be available in the evenings, even for non-emergency care. And we’re putting this burden on the segment of the workforce – mostly women in their 30s and 40s – that already has a heavy caregiving responsibility at home at night.
We wouldn’t ask this of dermatologists.

Care After Hours: Who Bears the Burden?
There are several aspects to this conversation. We have a talent pool who are primarily female who already disproportionately have a higher level of responsibility with parenting and home. Increasing evening hours makes care more accessible for children and families but creates challenges for the workforce.

Michelle Turner
Vice President, Clinical Talent and Delivery, Hazel Health
High Prime-Time Demand
There’s a huge increase in the demand, but what we’ve seen within the demand is that huge increase is between 4:00 and 7:00 PM. It makes sense; the majority of people work during the day and they’re always looking for after hours. So we struggle a lot with filling clients’ needs for therapy services because of the demand for that prime time. Monday through Thursday, 3-7 PM, we’re booked for months, but we have a 9:00 AM slot open probably every day.

Dr. Nefta Pereda, PsyD, MBA
Chief Program Officer, Radiant Futures

Solve clinical supervision for your organization
Access an underutilized and ignored portion of the behavioral health workforce. We’d love to show you how to make a real change.
6.
Supervision is Both a Recruiting and a Retention Tactic
Organizations recognize that supervision serves many important purposes. It’s essential for developing the next generation of therapists, acts as a valuable incentive to attract associates to meet the growing demand for care, and is considered both a privilege and an honor for those in supervisory roles.
Supervision: A Key Recruiting Lever
A lot of our workforce, about 90%, is pre-licensed. Covered supervision through Motivo is our big selling point on our sheet of benefits, because of the cost of supervision that people undertake.

Carla Myers, MS, LPC, MHSP
Former Clinical Director, Bridge Health
Fill their Cup, Feed their Passion
We have clinicians who are so passionate and want to make a difference in their communities, but also, they get burnt out, and let’s not forget, they’re practicing so there’s secondary trauma. So they want to change up what they’re doing. Maybe they became a manager, maybe they moved into quality assurance, maybe they’ve been moved to being supervisors. They want to advance and do different things. And those kinds of advancement opportunities work for retention.

Carla Myers, MS, LPC, MHSP
Former Clinical Director, Bridge Health
Supervision Bonus: A Retention Tactic
One thing we’ve done is that if you’re providing clinical supervision you get an extra quarterly bonus of $1000 per supervisor. We cap you at 2 to 3 supervisees per quarter. So it’s a nice little added bonus; it keeps people engaged, they get 2 hours of additional admin time every week to do it (one hour to do the supervision and one hour to do the co-signing of the notes to ensure fidelity to everything that’s needed). That has been a retention factor: It’s not just the cash, but it’s the time, and also it’s like an honor, like, hey I’ve been selected.

Rebecca Murray, LCSW
Senior Clinical Director of Behavioral Health, Oak Street Health


Managerial Responsibilities Help with Retention
We’ve found that folks get antsy after a few years. We actually just added another layer of leadership within our behavior health program to help us address our growth. The senior behavioral health specialist is a role that does 4 days of patient care and has one day of administrative time weekly to do the overseeing, making sure the behavioral specialists they cover are keeping fidelity to the model of collaborative care, educating the senior medical directors about what’s happening with the behavioral health program, doing a lot of onboarding, interviewing candidates to assess for clinical ability, and doing clinical supervision. And this has been a good retention factor.

Rebecca Murray, LCSW
Senior Clinical Director of Behavioral Health, Oak Street Health

A Clinical Management Advancement Track
We talk a lot about moving into management but there is also a clinical track where you can still feel like you’re advancing. You can become the in-house expert on something you’re passionate about, like, say trauma and kids. So you know that subject better than anybody; you have a niche, it makes you more marketable. And when younger clinicians come through, it’s nice to have somebody seasoned with that expertise and reputation.

Celeste Nevarez, MC, MPH, LPC-S
Chief of Clinical Services, Emergence Health Network
Making the Economics Work
Previously, I was able to take 20% of my staff’s time to let them teach, supervise, do research, quality compliance, whatever it was – and then I would still have a margin and I would give them a career path and the ability to do something different. It was really helpful because at the time I didn’t have the resources to be able to fund those positions but needed them and it helped me a lot with retention. I’m trying to recreate a little bit of that at Concert. The problem is with such a large workforce, we’re getting LMSWs, people that aren’t independently licensed, they obviously want to work towards licensure. What do we do with so many people who are then independently licensed? You have them at a higher pay scale, and if they want to do something outside of patient care, it becomes impossible to accommodate all of them because there’s too few opportunities, so you wind up losing a lot of them.

Virna Little, PsyD, LCSW-R
Co-Founder, Concert Health
Celebrate the Wins
We have a behavioral specialist who puts out a monthly newsletter and we ensure that we are highlighting anybody who we think needs a little boost; we need to help support their career.

Rebecca Murray, LCSW
Senior Clinical Director of Behavioral Health, Oak Street Health
7.
Organizations Need Trained Managers, but Struggle to Deliver
As the demands on mental health organizations continue to grow, there is an increasing recognition of the critical role management can play in running the organization smoothly and supporting the training, career development, and retention of therapists. Additionally, rewarding high-performing people with opportunities in management and supervision offers them a career path for advancement, and works as an incentive to remain with the organization.
However, while the benefits of moving people into leadership positions are clear, there’s a recognition that personnel management is very different from client management, which is what most people were trained for. And organizations don’t know how to teach these personnel management skills.
Management Growth with Organization Growth
At our smaller locations, there’s a sense of community, you probably know the client’s daughter / granddaughter / mother / there’s some connection. Our largest clinic is very transient, so people don’t have a sense of community or connection. This clinic is very hard to keep staffed simply because of the nature of how large it is. So I see my job being to help my managers make their job easier so they can help make the community support staff’s job easier – whether that’s looking at processes, how we can reduce documentation, getting more people, whatever it is to support them.

Carla Myers, MS, LPC, MHSP
Former Clinical Director, Bridge Health

Managers to Help with Career Pathing
It’s really important to me that our team feels a sense of purpose and variety in their work, especially when a full client schedule day after day can sometimes feel routine. Opportunities like supervising student interns, developing a training on a topic they’re passionate about, opportunities to learn a new skill, or starting a new group therapy can add valuable diversity to their day. As a supervisor, I aim to create space for these meaningful, creative activities that help keep our specialists motivated and fulfilled.
There’s got to be room for creativity and variety of work. But if they’re already overworked and burned out, they’re not going to think of these creative ideas. When our team is already stretched, adding responsibilities needs to be done thoughtfully. Instead of simply piling on more, it’s about rebalancing their workload to make room for these engaging opportunities. It’s my job as the supervisor to make sure that we’re giving our therapists the variety they need. I think that’s where managers get tripped up. I can’t be like, ‘oh, here’s a pizza party, make sure you’re self caring.’ It’s my responsibility and I think that makes a big difference. If you’re burned out, the idea of doing something else, even if it gives you variety, may feel like ‘what else do you want me to do?’ You need to take something off their plate. I can’t just be like here’s another full project for you to do. It’s a reallocation and a redistribution of work. But if you can get to that sweet spot and people are happy to come in, then I think they’ll do it with great conviction.

Celeste Nevarez, MC, MPH, LPC-S
Chief of Clinical Services, Emergence Health Network

Lack of Management Skills
People get promoted to be managers because they were good at delivering care to individual patients. But it’s not the same skill set to be a manager. And then they don’t get taught about how to be a manager of a program. There’s a lot of pressure to not be the person who has to say “hey, you’re not making the bar here.” That’s really hard to do. I don’t think we teach people how to do it well. Especially when somebody’s invested that much time and energy to get to that point, what are you gonna say? “I don’t think you’re safe to practice” after three years that somebody’s invested and how many thousands of dollars? But we do need ways to remediate so that we keep our patients safe.
I do think there are different sets of skills: How do you monitor people’s clinical service delivery and give feedback and do continuous quality improvement on the clinical care that they’re delivering. I think there are numerous challenges to this: people don’t have the skills and often don’t have the data.

Anna Ratzliff, MD, PhD
Co-Director, AIMS Center, University of Washington
Burned out Managers and Trainers
Managers and trainers are often burned out themselves. Providing therapy is hard, and it takes an emotional toll on the therapist. Just listening to story after story of children talking about their parents that abused them sexually or physically or otherwise, that’s hard to do for five straight hours a day; it’s very much a secondary trauma type thing.
The LMFT Model: Training and Supervision of Supervisors
I think LMFTs have gotten it right when it comes to supervisor training. I’m an LMFT, but I’m also an AAMFT-approved supervisor. I had to go through 30 hours of training to be a supervisor, and then I had to go through 18 months of supervision of me providing supervision. In most other disciplines, supervision training isn’t required or isn’t this intense. So what makes you as a clinician ready to provide clinical supervision if you’ve never had any training on how to actually prepare the next generation of clinicians? A lot of times it looks like, let me just tell you what I would have done as a therapist. That’s not really a supervisor’s role. A supervisor’s role is to help you become the clinician that you are meant to be, not to make you a cookie cutter of the supervisor.

Rachel Ledbetter, LMFT
CEO & Co-founder, Motivo Health
8.
Rather than Fight Attrition, CMHCs are Designing For It
For years, community mental health centers have addressed the issue of staff retention. They invest in training pre-licensed therapists, only to see them leave once they become licensed, forcing the organization to restart the whole process from scratch.
However, there is growing acceptance that this pattern is not likely to change, and organizations must now build it into their strategies. These organizations are deliberately starting to see themselves as a 2-3 year developmental ground where people come, following Graduate School, to partner with them, get their license, and move on.



Short-term employment: A deliberate strategy
We no longer consider ourselves a long term employer. We hire people who are new to the field and give them extra training, but we know that three years later they’re going to leave. We’ve tried so many things over the years to retain people, but we’ve essentially had to change our strategy and move away from a path to retain them. We can’t compete with the private practices, and we can’t give everybody a career path, so our goal is to equip them while they’re with us.

Dr. Nefta Pereda, PsyD, MBA
Chief Program Officer, Radiant Futures
I talked to a large outpatient mental health organization recently, with thousands of people. They said they no longer consider themselves a long term employer. They hire people who are new to the field, they give them extra training and they know three years later they’re going to leave. They don’t even have a path anymore to retain them. That is where they’ve shifted because they can’t compete with the private practices and they can’t give everybody a career path. They want people to stay but the reality is they know that a majority of the workforce is just going to churn at that level.

Virna Little, PsyD, LCSW-R
Co-Founder, Concert Health
Retention through Licensure
We accept that licensed clinicians do not stay in nonprofits long and that’s OK. So when we consider retention, we’re not trying to keep our licensed therapists working for half the pay that they can get somewhere else. Our retention strategy is to have them stay with us throughout the tenure of them acquiring the hours, so about two-and-a-half to three years; that’s the lifespan of a clinician in our mind. Some agencies don’t even keep them that long. So if it takes them three years to get their license, they might switch jobs once, maybe twice. But our retention efforts is to have them stick with us until they’re ready to go to the next phase of their life.

Dr. Nefta Pereda, PsyD, MBA
Chief Program Officer, Radiant Futures
Manage the Cost of Attrition (titrate up/down)
When we bring associates in, they are in the training and shadowing phase for the first 45 days. Then, little by little, they start getting their own cases. It takes about one to two months for them to get a full caseload. In that time they’re missing out on helping people. Then as folks leave, our clinicians don’t just walk out. They’re good; they give us six weeks or eight weeks’ notice because they love their clients so much. We’ll see them titrate down as well; they’ll stop getting new clients and just slowly start finishing their clients. At the beginning it takes about two months to titrate up to a full caseload and then the last two months they’re titrating down – so they’re not at full caseload for a couple months on either end. But we manage the overlap, so our capacity is not affected.

Dr. Nefta Pereda, PsyD, MBA
Chief Program Officer, Radiant Futures
9.
Private Practice Looks Greener, But May Not Be
All the organizations we talked to identified private practice as their biggest competitor. However, private practice has its own challenges. Despite the growing demand for mental healthcare, success in private practice is not guaranteed, and many clinicians are choosing to return to the security and support that organizations provide.
The Dubious Lure of Private Practice
We’re competing with private practice – it’s all over social media, which makes it look so much more attractive. People go to school to be a therapist because of what they see online, then realize that it’s actually much harder. They think, I’m going to have a schedule that works for me. But what we found is, people have left for that and then they come back a couple of years later saying, I really also liked having benefits. We’re finding people closing down their private practices and saying, I’m coming because I want the stable salary and I want the benefits.

Rebecca Murray, LCSW
Senior Clinical Director of Behavioral Health, Oak Street Health

Private Practice Has Gotten More Challenging
Private practice is much harder than it appears. It takes a great deal of business acumen that clinicians don’t typically have access to. Managing a private practice has become increasingly challenging, with the competitive landscape evolving significantly. Therapists now face more market competition, making it more difficult than ever to sustain a thriving private practice on dated assumptions. Honestly, community mental health is harder too: the work is heavier and there’s more competition for CMHCs. Five years post COVID, the wave of people seeking virtual therapy is dipping down closer to pre-COVID levels – those who were in virtual practice during the pandemic now face the challenge of adapting to decreased demand and competition with hybrid or in-person services that some clients are preferring as they seek more personal connections in their therapeutic experiences. Potential clients often perceive therapists sharing advice on their YouTube channel as being in tune with the latest treatment or trends, which makes them more appealing. In contrast, therapists who are less active or savvy on social media can face challenges connecting with their ideal client to build their practices.

Carla Smith, PhD, LCSW, LMFT
Chief Clinical Officer, Motivo Health
Owner, Haven Therapy and Wellness
10.
We Cannot Adequately Support the Next Generation of Therapists
If we don’t hire associates, they won’t become licensed therapists, and we’ll never get out of the supply crunch that we’re in. And yet. And yet and yet and yet, despite this pressing need, there are still issues around hiring associates.

A Two-Class System that’s Bad for Everyone
Commercial insurance for the most part doesn’t allow you to bill for associate level therapists. This is what draws new therapists to community mental health organizations, where they can bill Medicaid for associates. So it’s a two class system: We treat Medicaid patients who have the more acute need differently. We use our greenest clinicians to serve the most vulnerable population. We give them very little training, and we’re like, good luck. If anything, it should be the reverse.

Rachel Ledbetter, LMFT
CEO & Co-founder, Motivo Health
State Differences in Reimbursement
One of the biggest challenges I see in the behavioral health industry is the way reimbursement works for pre-licensed therapists – and it’s different in every state. In some places, Medicaid and private insurers won’t pay for services provided by pre-licensed therapists, even when they’re being supervised by a licensed clinician. This creates a real financial burden for behavioral health organizations. It makes it harder for them to hire, train, and support new therapists, which leads to staffing shortages, burnout, and higher turnover. Ultimately, this hurts everyone – the clients who need care, the organizations trying to provide it, and the next generation of therapists trying to get their start. If we want to build a strong, sustainable mental health workforce, we have to address these reimbursement gaps. It’s not only about paying people fairly – it’s about ensuring access to care and supporting the future of this field.

Carla Smith, PhD, LCSW, LMFT
Chief Clinical Officer, Motivo Health
Owner, Haven Therapy and Wellness
Unproductive Stigma Around Associates
We have a really awesome opportunity for masters level individuals who are seeking their pathway to clinical licensure. We were hoping to have at least 20 fellows this year; we’re short, we’re only at 13. My hope is that we’re able to continue to show the validity of this program. But it’s hard to convince our medical directors and our regional vice presidents to staff a fellow. They think ‘oh, this person doesn’t have clinical training, they’re not prepared, I don’t want them working with my patients, I want someone fully licensed who’s done the work and I don’t have to worry.’ So we are working with the stigma of it, and that’s one we definitely want to address.

Rebecca Murray, LCSW
Senior Clinical Director of Behavioral Health, Oak Street Health


In Need of a Rebranding?
There is still this stigma that if you’re not licensed you don’t know what you’re doing versus if you’re licensed that means that you’re knowledgeable. We tell our clients that all our therapists are pre-licensed, it’s in our consent. We need to share the supervisor’s information with the client just in case something does come up, they know where to go. We let them know it’s like a driver’s permit so there’s always someone over 25 in the car when they’re driving. So the clinical supervisors – that’s our Motivo clinical supervisors – know about the cases, and they consult with them on the cases; so there is a licensed driver in the vehicle with them. I mean it literally is like residency and medical school but they’re called residents so it sounds cool and here we call them pre-license which just sounds less authoritative.

Claudia Flores, LCSW
Director of Clinical Services, Radiant Futures


The Harsh Realities of Being an Associate
I have 6 associates under my license whom I’ve been mentoring in my private practice. I hear feedback from them all the time that being an associate is extremely challenging. You’re not making very much money. You have a lot of pressures. Your student loans have come up for repayment and you also need to make enough money to live and earn hours for your license. Most associates are working more than one job to make ends meet. It’s extremely challenging and I think that most associates feel like that whole setup is very unfair.

Adina Ascher, LCSW, PhD
Clinical Director, The Liberation Institute
Conclusion
We simply cannot expect to meet the demand for mental health services with well-prepared therapists unless we dramatically shift course, and invest meaningfully in the training and well-being of the next generation of mental health professionals. The current model, with its lack of support, trial-by-fire training, and financial barriers, is unsustainable.
This shift begins with changes in education and training, at the university and the practicum and pre-licensure stages. Students entering the field deserve structured, comprehensive training under the guidance of healthy, skilled supervisors, rather than being thrown into high-stakes environments with minimal oversight.
The double-tiered reimbursement system—where services are often undervalued for Medicaid patients compared to private insurance—places new therapists in high-pressure situations that often leave them without adequate preparation or support. Bridging this gap, so that new therapists don’t have to worry about unpaid or underpaid internships, will be critical to creating a fair and effective training system for all aspiring therapists.
For our practicing therapists, we must learn how to prioritize employee wellness and professional development, since a burned-out therapist cannot provide either effective care or effective training. By focusing on building a culture of growth, we can retain skilled professionals and, importantly, offer better services to the communities who depend on them.
Ultimately, a revolution in training will require collaboration across educational institutions, mental health employers, and policy-makers. If we commit to these changes, we can foster a new generation of mental health professionals who are equipped, supported, and inspired to meet the needs of the communities they serve.
About Motivo
Motivo Health is a leading provider of virtual clinical supervision dedicated to supporting therapists throughout the licensure process.
With a core mission to address the shortage of licensed mental health providers, Motivo has helped over 5,000 aspiring therapists obtain the hours needed to become licensed therapists. Motivo has built a network of over 1,200+ vetted, high-quality clinical supervisors across all 50 states and partners with over 130 organizations to provide remote clinical supervision to their pool of associate-level clinicians.
We partner with behavioral health organizations of all sizes including treatment centers, health plans, digital health companies, government programs, and more.

Have your voice heard.
What are the trends impacting your business or workplace the most? We value your feedback & your response will be kept confidential.
